Information for Patients
Patient Information Leaflet
Click on the link below to see our Patient Information Leaflet;
Responsible GP
All patients registered with a GP in England must have a named accountable GP. This is a largely an oversight role and the accountable GP has the responsibility for co-ordinating all the services that patients are entitled to under the partnerships contract with the NHS. They ensure that these services are available if needed by the patient. This does not mean that that doctor is the only doctor available to provide care and a patient is still able to see any GP they like at the practice.
At SHP, the partnership board has delegated authority from the partners to oversee the delivery of services. The board is made up from 5 GP partners and has a chairperson. It is the chairperson who is the named responsible GP for patients at SHP. The current chairperson is Dr Arturo Lupoli.
Our Doctors
Dr Tahiraa Afzal (f)
Dr Shadan Alam (f)
Dr Michelle Caughey-Rogers (f)
Dr Beverley Dickinson (f)
Dr Deborah Edwards (f)
Dr Mark Fernando (m)
Dr Maria Font (f)
Dr Bhavesh Gandhi (m)
Dr Simon Green (m)
Dr Barbara Guilfoyle (f)
Dr Bayan Hariri (f)
Dr Sunil Kotecha (m)
Dr Kapil Lad (m)
Dr Shamah Mahmood (f)
Dr Nish Patel (m)
Dr Charandeep Sadhra (m)
Dr Nicola Sawle (f)
Dr Fatima Tahir (f)
Get Help Sooner
Our Care Navigators are trained to get you to the right person first.
Don't be offended if they ask you about your condition when you request an
appointment.
They may suggest a professional who can see you more quickly than your doctor,
such as:
- Minor Eye Conditions Service
- Dentist
- Talking Therapies
- Community Pharmacy
- Social Prescribing

What is prostate cancer?
Prostate cancer can develop when cells in the prostate start to grow in an uncontrolled way.
Some prostate cancer grows too slowly to cause any problems or affect how long you live. Because of this, many men with prostate cancer will never need any treatment.
But some prostate cancer grows quickly and is more likely to spread. This is more likely to cause problems and needs treatment to stop it spreading.
Signs and symptoms
Prostate cancer that’s contained inside the prostate (called localised prostate cancer or early prostate cancer) doesn’t usually cause any symptoms. That's why it's important to know about your risk.
But some men might have some urinary problems. These can be mild and happen over many years and may be a sign of a benign prostate problem, rather than prostate cancer.
Find out more information about the possible symptoms of prostate cancer.
If you think you might be at risk of prostate cancer or are experiencing any symptoms, visit your GP or speak to prostate cancer UK Specialist Nurses.
If you’re not sure about what to say to your GP, print and fill out this form and show it to them. This will help you have the conversation.
Are you at risk?
In the UK, about 1 in 8 men will get prostate cancer in their lifetime.
https://prostatecanceruk.org/risk-checker
Prostate cancer mainly affects men over 50, and your risk increases with age. The risk is even higher for black men and men with a family history of prostate cancer.
Facts and figures
Below are some of the very basic facts and figures about prostate cancer.
(Last updated: August 2023 To be reviewed: August 2024)
Across the UK
- Prostate cancer is the most common cancer in men.
- More than 52,000 men are diagnosed with prostate cancer every year on average – that's 144 men every day.
- Every 45 minutes one man dies from prostate cancer – that's more than 12,000 men every year.
- 1 in 8 men will be diagnosed with prostate cancer in their lifetime.
- Around 490,000 men are living with and after prostate cancer.
Click on the link below to access further information
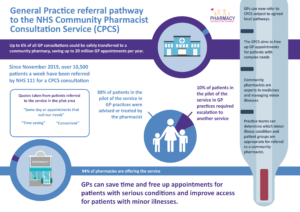
Community Pharmacist Consultation Scheme
SHP participate in an approach to improve access for patients to GP appointments. The aim is to direct patients to the most appropriate healthcare professional, which may be a GP or a pharmacist.
If your symptoms could be resolved by a booked consultation with your local pharmacist instead of the GP, you will be given a same-day referral to a local community pharmacy.
SHP takes part in the Community Pharmacist Consultation Service (CPCS), which includes Astwerwell Pharmacy in Shirley and is expanding to more community pharmacies local to our surgery sites.
We think this is a good thing. Once you see how great your local pharmacist is – they are highly trained and skilled clinicians experienced in treating minor illnesses – we don’t think you’ll look back.
This will also help us to free up GP appointments for people with more complex health needs and ensure that everyone gets treated at the right time, by the right healthcare professional.
We are keen to hear what you think and will be listening to your comments and feedback about your experience of using this service.
You can give comments and feedback - Click Here
Prescribing of over the counter medicines
Patient guide: Steroid Emergency Card (SEC)
Why have I been given this card?
You have been given the NHS Steroid Emergency Card as you are taking long-term steroid treatment. It is important that any healthcare professional who treats you knows you are on long-term steroids. You should not stop suddenly taking your steroid treatment, as you may feel very unwell if this happens. You could have weakness, dizziness, tiredness, feeling or being sick, poor appetite, weight loss and stomach pain.
What do I need to do?
You must complete the card with your own details. Keep it safe in your purse or wallet.
Have it ready to show any healthcare professional you see.
Please let your family know that you carry a NHS Steroid Emergency Card. Ask them to remind you to show your card at every chance when getting treatment. This is very important if you need emergency treatment, they can tell the emergency services for you.
Do I still need to keep the blue Steroid treatment card too?
Yes, you will need to keep both, however the new NHS Steroid Emergency Card is very important. Also still wear your medic alert bracelet or necklace, and keep any other emergency cards you may have.
I have lost my new card, where can I get another one from?
New or replacement NHS Steroid Emergency Cards can be obtained from your community pharmacy, hospital or GP practice. You can have more than one card if you would like to store them in different places. Please make sure the details on both cards are the same. You can also screen shot the NHS Steroid Emergency Card and save your card. Then you can have it as screen saver on your smart phone. See further advice on how do this at: Steroid Emergency Cards | Addison's Disease Self-Help Group (addisonsdisease.org.uk)
Steroid Emergency Card (SEC) – what it looks like:
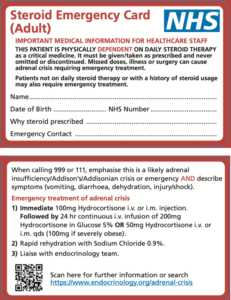
The link below is a direct link to the online steroid card.
How to access us and ask for help?
We are still open and here for you. We are continuing to provide services as we have been doing throughout the pandemic, and prioritise delivering care and services based on clinical needs.
If you need medical advice or treatment, please call us on 0121 705 1105 or, for non-urgent advice or treatment, visit our website or one of our surgery sites.
By Phone
You can call us on 0121 705 1105. Our telephone lines are open from 8am to 6:30pm, Monday to Friday (excluding Bank Holidays).
You will be asked to first discuss your condition/s over the phone with a trained Care Navigator to assess the most appropriate way to provide your care, which may include a face-to-face consultation, and ensure it is provided by the most appropriate person.
In person
You are able to access us face-to-face by visiting one of our surgery sites to ask in person about booking an appointment, repeat prescription requests and for general queries.
From Monday 8th November 2021, our sites will be open from 8:30am to 6:30pm, Monday to Friday (excluding Bank Holidays):
- Shirley Medical Centre
- The Jacey Practice
- Haslucks Green Medical Centre
- Grove Surgery
- Monkspath Surgery
- Dickens Heath Medical Centre
This ensures we are able to prioritise our focus on patients being able to access us through our telephone system when the demand is at its highest and support improving patient access for the majority of patients.
All sites will continue to be closed on Wednesdays from 12:30pm to 1:30pm, as part of our ongoing staff training and development, which is a priority to ensure we continue to improve service delivery and patient care. We are also dedicated to continuing to further upskill our Care Navigators with a programme of additional training and development to support our clinicians, and to ensure our patients see the right healthcare professionals at the appropriate time.
Our telephone lines remain open throughout the training and in the event of urgent patient needs, we can still be contacted. There is minimal impact on service delivery and no impact on appointments. This time has been chosen to coincide with the period of the day when our Doctors and healthcare professionals are conducting essential face-to-face appointments with housebound patients.
We continue to have a range of measures in place to keep you safe from COVID-19, including regular cleaning of patient areas and social distancing. Please ensure you wear a face covering when visiting us at one of our sites. If you have a disability or condition which means you cannot wear a face covering or cannot communicate with someone who is wearing a face mask, or require other adjustments before your appointment, please let us know ahead of your arrival.
Individuals with cough, cold or flu like symptoms, COVID-19 symptoms or who meet criteria for self-isolation, should not attend our surgeries and stay at home. You should continue to follow public health guidance and if you have a clinical need your appointment will be by telephone or video, for patient and staff safety.
Please be polite and respectful, our GPs and practice teams are available and working hard to support you, your family and friends health and care needs.
Go online
Online services currently provide patients with access to their medical records, repeat medication ordering and COVID-19 vaccination status. Using the service will help you to manage your own health and access healthcare features whenever you need to.
You can visit our web site, and order repeat prescriptions and access your medical records on the NHS App and Patient Access – To access and find out more visit: https://solihullhealthcarepartnership.nhs.uk/online-services/
Our Online Consult facility is currently unavailable for patient safety online and clinical governance reasons. We are in the process of reviewing our online services to improve patient access and services, and will keep patients updated via our web site and social media.
Did you know?
You can visit your local pharmacy (Find a pharmacy - NHS (www.nhs.uk) for clinical advice on minor health concerns.
And for urgent issues or out of hours, you can also call the NHS on 111 or go online to seek NHS advice 111.nhs.uk (NHS 111 online)
Our staff are continuing to work extremely hard to provide services and care, and we would like to thank our patients for your continued support.
#HelpUsHelpYou
TRAINING:
We are committed to training healthcare professionals at SHP. Being a training practice means that we have Specialist Trainees (STs) and Foundation Doctors (F2s) working in our team.
All are fully qualified doctors – the ST Doctors are training to become GPs, and the F2 doctors are doing more general training in the second year after qualification as doctors.
We also sometimes have medical students sitting in on consultations as part of their educational process. Your support in this is very much appreciated. We always ask your consent for this and if you prefer the student not to be present, your care will not be affected.
Why was SHP formed?
Solihull Healthcare Partnership (SHP) was formed in October 2018 and moved to a single registered practice in October 2019. In line with the NHS long-term plan, SHP was created as a single site primary care network (PCN). There are countless benefits to being a PCN, if you would like to read more, please visit: https://www.kingsfund.org.uk/publications/primary-care-networks-explained#what-does-it-mean-for-patients
