Latest News
COPD patients invited to join research study
There is a new study taking place at University Hospitals Birmingham (UHB) looking at Chronic Obstructive Pulmonary Disease (COPD), and Solihull Healthcare Partnership will be identify patients suitable to take part in the research.
Patients can help with research into a drug which may reduce the number of episodes of worsening COPD (flare-ups).
Invited patients will meet the following criteria;
- 40 – 85 years of age
- Will have had COPD for more than 12 months
- Will have had at least 3 flare-ups in the last 12 months
- Is taking regular medication to manage their COPD?
The clinical study is being carried out with patients with moderate to very severe Chronic Obstructive Pulmonary Disease (COPD), and is being conducted to see if a new precision drug called benralizumab can help control COPD better if it is added to available COPD inhaled medications.
SHP will identify suitable patients and contact them directly to see if they are willing to take part in this study, where they will then be contacted by the University Hospital Birmingham research team.

Young People Visit the Practice to Improve the Patient Experience...

Photograph of Damian King (Project Lead), Lisa Hall (Care Navigator at SHP) and three 'Experts by Experience' (Our Voices Heard) at Haslucks Green Medical Centre.
Measles: Are you protected?

Healthwatch Solihull
If the costs of things like food, medicine and heating are worrying you Healthwatch Solihull has put together a list of local organisations that can help. https://healthwatchsolihull.org.uk/cost-of-living-crisis/
For more information contact 0808 196 3912 or enquiries@healthwatchsolihull.org.uk

An Introduction to eConsult, our Online Consultation Platform…
In our continuous efforts to improve the patient journey and the way we provide healthcare services, Solihull Healthcare Partner (SHP) were delighted to announce in November 2023 that we went live with a new online consultation platform.
What is online consultation?
Online consultations allow a patient to submit their request via an online form, as an alternative to calling us or visiting one of our surgery sites. The patient will be asked questions and submit answers to their specific health query or concern, which will then be sent to the practice.
The information provided will allow us to ensure the patient can access the care they need from the right healthcare professional or service at the most appropriate time.
What is eConsult?
eConsult is an NHS-approved digital triage tool designed to enhance patient access, improve practice efficiency and support our fantastic care navigation team (supervised by a dedicated GP) in signposting patients to the right place at the right time for their care.
Developed and managed by NHS doctors, eConsult is one of the leading online consultation platforms in the NHS. Available through our website or the NHS App, this tool offers a clinically safe method to submit patient information.
We want to make sure patients are getting the advice they need at the right time from the right person the first time they contact us about that medical issue.
Having completed a review and investigated, with our Digital Transformation Lead, all available new technology and digital access tools to facilitate an expansion of the digital offering for our patients, we believe eConsult is the best online consultation option.
Benefits of eConsult
Ease of access.
Allows the patient to ensure their concerns are described in full.
Same day response (Monday-Friday).
How to access eConsult
The initial launch today, 8th November 2023, is the first phase of eConsult, and will allow us to review and evaluate the processes and ensure our practice team are performing efficiently. This stage will be shortly followed by a next phase in the coming months.
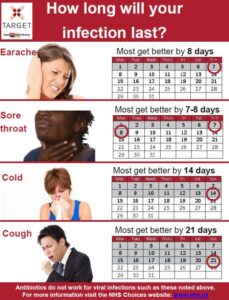
At this initial stage whilst we are reviewing the processes, we ask that patients use the service for administrative queries and acute illnesses only (an illness with recent onset, usually of short duration and not considered a long term condition, such as a cough, cold or sore throat).
The service is available between 8am and 10am, Monday to Friday, and is limited to 100 completed forms per day.
You can access eConsult by clicking the link below or directly via the NHS App if you are an existing user.
https://solihullhealthcarepartnership.nhs.uk/econsult
What happens once we receive your submitted form?
All forms are reviewed by our care navigation team, which includes a GP, once they are received. This will then lead to an assessment of next steps needed in patient care. We will deliver a response by 6.30pm the same day and may be sooner, especially where an urgent assessment has been required.
FAQs
Is my data safe?
eConsult is a data processor, they collect patient information and pass it onto the practice in a format that makes it easy for the practice to read. Once they have passed it to the practice (usually in a matter of seconds) eConsult delete any identifiable patient information. eConsult are not here to sell your data.
Can I submit an eConsult for someone else or my child?
As a parent or guardian of a child between the ages of 6 months to 16 years, you will be able to submit eConsult forms about symptoms or conditions. Patients using the eConsult service should submit forms based on their own symptoms or conditions.
In some cases, it may be likely that people need help submitting an eConsult, perhaps because they cannot access or are not comfortable using services online. You have a route to enable you to submit on behalf of someone else who is registered at the practice and will require their consent.
What about patients who are not able to use eConsult?
If you are not able or would prefer not to use eConsult, all usual methods of access continue to be available to patients, including telephone and visiting us at our surgery sites.
Does using eConsult mean I will get an appointment?
No, however it will ensure the patient can access the care they need from the right healthcare professional or service at the most appropriate time.
Has there been any patient involvement in developing the online consultation platform for SHP?
Yes, our Patient Participation Group have tried and tested eConsult and our processes prior to the launch, providing us with vital feedback to help ensure it is user-friendly and a positive the patient experience.

An image of a person using a mobile phone showing text and accessing the eConsult online consultation form.
Fancy a Chat?
NHS Volunteer Responders are there to offer you or someone you know a friendly phone call and a listening ear through their newly launched Check In and Chat service.
Whether it’s just a one-off conversation, or regular chats, you can use this service by calling 0808 196 3646.

A Day in the Life of… a Care Navigator
My name is Cathrina and I’m a Care Navigator at Solihull Healthcare Partnership.
The 84-year-old pensioner possibly having issues with addiction to controlled drugs, a mum with an unwell five year-old child, an agitated patient who has run out of anti-depressants and a bereaved family reporting the death of a loved one.
These are just some of the calls that I received in one day as a Care Navigator with Solihull Healthcare Partnership – the largest GP partnership in Solihull, providing care to more than 55,000 patients across six surgery sites.
My typical day runs from 12.30pm until 6.30pm, and it’s an intense afternoon of back-to- back calls from the physically and sometimes mentally, unwell. My role and that of my colleagues, is to listen and safely signpost patients to the most appropriate source of help provided by SHP which can include their GP, a community pharmacist, nurse, minor operations or other community services such as sexual and mental health services.
Many of the calls we receive at our hub based at Shirley Medical Centre may not require the services of a GP, and our role as specially trained Care Navigators is to help ensure patients see the most appropriate healthcare professional or service for their needs.
Loneliness and heartache can’t be cured with a prescription however and it’s a sign of the times that so many of us are suffering with our mental health.
Often the elderly or vulnerable person who has called to see their doctor also wants to just talk.
I took a call from a 94-year-old lady who was also the carer for her husband who had dementia. She couldn’t walk far so found it hard to drop off her repeat prescriptions at her local surgery.
She didn’t have access online and didn’t like to ask either of her daughters for help. She was able to ring us though so it was important to reassure her that her medication would be sent to her pharmacy in good time. But it was also a chance to ask if there was anything that we could help her with and if the surgery's social prescriber could offer assistance.
At the other end of the scale, I had an anxious mum who was worried that her son's had a sore bottom which turned out to be worms. It was a simple case of popping to her nearest pharmacy to obtain medication to treat the whole family, therefore saving a GP appointment for someone more in need.
Many of my calls are patients following up the results of blood tests and referrals or are requesting repeat prescriptions. Some are worried that their pharmacy has not got a particular medication in stock. We can seek the advice of our in-house pharmacy and pharmacy technician team - pharmacists are highly qualified medical professionals with at least five years of training.
Answering the hundreds of calls each day is often like opening Pandora's Box; suicidal patients who are urgently dealt with, a newly pregnant woman booking her first midwife appointment or a call from a Marie Curie specialist nurse dealing with the final days of a patient's life.
It's astoundingly busy and we often bear the brunt of people's frustrations, but helping patients to live their best life is so rewarding and I wouldn't swap my job for the world.
A Day in the Life of… a Physician Associate
My name is Farzana Islam, also known as Sylvia (there is reason for using my middle name but you’ll have to ask me the story when you see me). I am the Physician Associate at Solihull Healthcare Partnership (SHP). I started in June 2020 and have mainly been a part of the acute care team supporting with telephone triage calls alongside GP’s, Advanced Nurse Practitioners, Clinical Pharmacists and Care Navigators.
Many people ask me, what is a Physician Associate? My role supports doctors in the diagnosis and management of patients. I am trained to perform a number of roles including assessing and taking medical histories, performing examinations, analysing test results, and treating and managing acute problems and illnesses in children and adults.
Prior to joining SHP, I started my career as a Registered Nurse in Solihull Hospital’s Acute Medical Unit and then moved to Birmingham Heartlands Hospital A&E department where I met some Physician Associates that got me interested in the role.
I trained as a Physician Associate and on graduating worked in both Secondary Care (Acute Medical Unit/Accident & Emergency) and Primary Care, following which I then worked in a General Practice in Birmingham for over a year.
My typical day starts at 8am with telephone triage calls, which can be everything from patients with chest infections, urine and ear infections to mental health and more – no one day is the same!
Today, for example, I called an urgent ambulance for a very unwell seven-month old baby to go to hospital, admitted a patient to hospital with a suspected Pulmonary Embolism, and gave urgent support to a patient suffering with mental health decline and liaised with the mental health crisis team.
I also have face-to-face consultations following the initial telephone consultations - this can vary depending on the calls we receive on the day and their presenting complaints – and I contact patients to follow up from their recent consultations to find out how they were progressing and if they needed any further treatment.
Due to the latest COVID-19 restrictions, and to protect vulnerable patients and staff members, I also see patients with suspected COVID-19 in the Ambulatory assessment Unit or on a designated car park area on surgery sites. This allows us to ensure they were seen and assessed for how unwell they were and if they needed referring for further treatment and urgent care at hospital.
My typical day also includes working with the pharmacy team and duty ‘on call’ doctors to assess acute patients contacting us with their on-the-day needs, and playing a key part in the team that delivers acute care for patients.
In between patients, I review blood test results, swabs and other investigations, as well as referrals, and go through hospital letters from Consultants to review if any further action is required for the patient as follow up.
It’s a great role and I love being able to provide care for our patients. At the beginning some patients were sceptical of my role and just wanted to see a GP, however once I’ve explained who I am and what I can do, I’ve had nothing but great feedback from patients.
A Day in the Life of a… General Practitioner
Hi, my name is Dr Behl and I’ve been a GP Partner at Solihull Healthcare Partnership (SHP) since 2018.
I’ve been a doctor for thirteen years and a GP for six years. After qualifying from Leicester Medical School, I have worked across the Midlands in different medical specialities before deciding on a career in General Practice.
Although I initially set out to be an acute medical physician, I was finding the pace of hospital life and the quick turnaround of patients on the wards dissatisfying. I was longing to build relationships with patients, following them on their individual journeys and providing the continuity of care which is the cornerstone of General Practice.
I have since developed a clinical interest in Rheumatology, working in a Community Rheumatology Clinic in Birmingham, having completed a postgraduate qualification from the University of South Wales. I assess patients with a variety of joint and muscle conditions, such as Rheumatoid Arthritis, Lupus and Fibromyalgia, amongst many others. Once again, I see patients from all ages and walks of life, sometimes with quite complicated disease which makes this a particularly interesting speciality. The interplay of disease and how this impacts a patient in their home, work and personal relationships is extremely important and with my GP hat on, I feel I can provide a holistic approach to care.
As a GP Partner here at SHP, I am also very involved with all aspect of running a large practice and this is extremely important. Being able to have a career which balances clinical care along with organisational responsibility keeps me intellectually stimulated to remain passionate about general practice and providing the best possible care to our patients.
I also have roles at Birmingham and Solihull Integrated Care Board within the Workforce team, primarily focussing on recruitment and retention of GP’s at a time where there is a significant shortage of GP’s within the UK. To overcome this, we offer a variety of schemes and programme which I oversee and deliver.
My typical day at SHP will involve starting early at 8am, reviewing my clinics of the day and to see which patients have been booked in and whether any home visits have been allocated. Before the clinic starts, I like to authorise prescriptions and review blood results, but this is not always possible due to the sheer volume of work we deal with.
At 8.40am clinic starts, and this can be a combination of telephone, video and face-to-face consultations, which runs right through to midday. The common conditions we deal with are mental health concerns, which has seen a huge surge since the pandemic, but also musculoskeletal issues, minor illnesses, alongside performing medication reviews and reviewing patients with long term conditions such as diabetes. No two days are the same, which makes it really interesting! Also having the pleasure of consulting with children as well as the elderly, or those patients in pain or in anguish means I am constantly changing and adapting my consultation style and approach throughout the day.
Once clinic is done, I will go and do any home visits if allocated, but if not I will use this time to do the referrals from morning clinic, complete my prescriptions, review blood test results and review letters that we receive from hospital clinics or other health professionals. This does generate a lot of work and tasks, and may involve further phone calls to patients.
I then prepare for afternoon clinic, which usually consists of more ‘urgent on the day’ appointments, which have been triaged by the on-duty team, and planned care appointments, which takes me all the way through to 6.30pm. I usually then continue into the evening to complete any outstanding actions and tasks for follow up from the day, as well as planned care such as reviews for certain groups of patients, including patients with cancer or learning disabilities.
Every day brings with it new challenges, but that’s what makes it such a rewarding job, and every day I enjoy delivering the best care I can to our patients.
A day in the life of… A Service Delivery Manager
Hi, my name is Natasha. I am a Service Delivery Manager at Solihull Healthcare Partnership (SHP) and I’ve worked in general practice for over nine years.
I started in February 2013 as an Apprentice Receptionist at Monkspath Surgery, which I completed within a year, and then became a permanent Receptionist/Administrator. After a few years I became a Senior Receptionist and in 2017 I completed a diploma course in care leadership and management at University.
In 2019, when SHP was formed, I went on to become a Senior Care Navigator and then progressed to become a Management Support Officer in 2020.
I’ve been in the role of Service Delivery Manager since May 2022, and look after two of our surgery sites, Monkspath Surgery and The Jacey Practice. Within the teams at my two surgery sites, there are Care Navigators, Doctors and Nurses, that all help with all patient appointments, whether it’s face-to-face or telephone appointments.
My role as a Service Delivery Manager is a new role at SHP primary care network and is a very varied one, no one day is the same!
My typical day starts at 7.45am, making sure my surgery sites are ready to open at 8.30am, that all the team are on-site and that any sickness cover is arranged, which can sometimes mean I’m covering for a Care Navigator on reception at one of the sites. Working alongside two other Service Delivery Managers covering our other surgery sites, we all ensure the rotas for both clinical and non-clinical teams are achieved.
A typical day also includes working with our HR, Governance, Finance and Communication teams to ensure that all colleagues and patients are updated regularly, as well as supporting with the training needs of the team, especially with new employees.
I also meet with clinical colleagues to discuss care plans with external providers such as District Nurses, Marie Curie and Macmillan Nurses, to ensure we are all providing the best care packages for any terminally ill patients.
As well as ensuring the teams are on-site, I regularly monitor and inspect my surgery sites to ensure that all facilities are in working order, that we comply with all health and safety standards, and that we are monitoring infection control.
Every day is different as a Service Delivery Manager and it can be very challenging, whether that’s helping a patient that’s collapsed in the surgery, supporting a blue light ambulance arriving on-site for a patient or managing staff sickness and dealing with the IT computer systems or internet access.
What I enjoy the most every day is being able to help and support our patients and everyone that I work with, problem solving and finding new ways to improve our patient experiences.
I love to see colleagues that I’ve trained progress in their careers and feeling like I’ve helped them along the way, as well as seeing a patient say thank you to one of our Care Navigators, Doctors or Nurses, and to know that we have provided the best care for the patient and have achieved something together. When it comes to the end of day, for me knowing that both our team and patients are happy makes all the hard work and long hours worthwhile.
Whilst the past three years have been tough for everyone and the challenging times continue, I hope that as Service Delivery Manager here at SHP I can continue to support and help my colleagues and patients, and bring back some happiness in the NHS.
A Day in the Life of a Governance Officer
Hi, my name is Gaynor and I am a Governance Officer at Solihull Healthcare Partnership (SHP).
I have been with SHP for just over a year and a half, and in that time I have had many duties within the organisation, including setting up the governance for and subsequently working at, the very first COVID-19 Vaccination Centre Clinic at Monkspath Surgery back in December 2020, which was ground breaking and I was proud to play a part in.
Since graduation, I have worked in many different industry sectors including IT and Postgraduate Medical Education, before joining the NHS in 2019. My role at that time involved co-ordinating the Extended Access and Anticoagulation programmes across North and South Solihull, where I was first introduced to SHP!
So, what is Governance in healthcare?
It is referred to as clinical governance, “a system through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish”. It involves monitoring systems and processes to provide assurance of patient safety and quality of care across the organisation.
In General Practice, the Care Quality Commission states governance is a systematic approach to maintaining and improving the quality of patient care and service delivery. It should be given a high priority by all healthcare providers.
As Governance Officer my role is very varied, for example yesterday I was updating our intranet with very important Safeguarding information following the Safeguarding Network Leads Meeting. This included research into the importance of engaging male carers in the prevention of non-accidental injury of children under the age of 1. Today, in conjunction with our new Service Delivery Managers at SHP, I am in the process of writing site information sheets for new colleagues joining the team. Even though all of our sites are based on a standardised operating model, there are subtle differences at our surgery sites, such as where the Fire Marshall jackets are kept.
A key part of my role is also distributing policies via our intranet to colleagues across SHP, which are ever changing due to changes in our processes to improve delivery and/or legislative requirements. For example, we have just received new Information Governance templates from our Data Protection Officer, which I am updating and distributing for SHP.
It’s important that we keep our patients up to date too and one really great way of doing this is via the surgery site noticeboards. One of my responsibilities is to keep these up to date with legislative requirements, such as liability insurance certificates, CQC registration, ICO certificate and Data Protection Policy, as well as health and safety information such as Fire Meeting Point and our Zero Tolerance Policy. We have recently had an emphasis on Abuse and reporting this, along with support pathways for those patients who may be in abusive relationships. We also display NHS Monthly Campaign posters on our patient boards, for example this month it was Chest Pain – Dial 999, and last month it was Cervical Screening and the importance of making timely appointments for check-ups.
As governance is a high priority for SHP, my role is a busy one, but one that I really enjoy. It is great to be part of a team that provides an effective governance framework to support the delivery of good quality care to our patients.
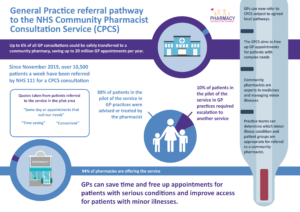
Community Pharmacist Consultation Scheme
SHP participate in an approach to improve access for patients to GP appointments. The aim is to direct patients to the most appropriate healthcare professional, which may be a GP or a pharmacist.
If your symptoms could be resolved by a booked consultation with your local pharmacist instead of the GP, you will be given a same-day referral to a local community pharmacy.
SHP takes part in the Community Pharmacist Consultation Service (CPCS), which includes Astwerwell Pharmacy in Shirley and is expanding to more community pharmacies local to our surgery sites.
We think this is a good thing. Once you see how great your local pharmacist is – they are highly trained and skilled clinicians experienced in treating minor illnesses – we don’t think you’ll look back.
This will also help us to free up GP appointments for people with more complex health needs and ensure that everyone gets treated at the right time, by the right healthcare professional.
We are keen to hear what you think and will be listening to your comments and feedback about your experience of using this service.
You can give comments and feedback - Click Here
What is a maternity link support worker and how do they help patients?
Take the worry out of weaning...
We’ve got top tips for parents:

NHS Healthy Start

A Message on behalf of Solihull Healthcare Partnership Patient Participation Group (PPG):

How to access us and ask for help?
We are open and here for you. We are continuing to provide services, and prioritise delivering care and services based on clinical needs.
If you need medical advice or treatment, please call us on 0121 705 1105 or, for non-urgent advice or treatment, visit our website or one of our surgery sites.
By Phone
You can call us on 0121 705 1105. Our telephone lines are open from 8am to 6:30pm, Monday to Friday (excluding Bank Holidays).
You will be asked to first discuss your condition/s over the phone with a trained Care Navigator to assess the most appropriate way to provide your care, which may include a face-to-face consultation, and ensure it is provided by the most appropriate person.
In person
You are able to access us face-to-face by visiting one of our surgery sites to ask in person about booking an appointment, repeat prescription requests and for general queries.
Our sites are open from 8:30am to 6:30pm, Monday to Friday (excluding Bank Holidays):
- Shirley Medical Centre
- The Jacey Practice
- Haslucks Green Medical Centre
- Grove Surgery
- Monkspath Surgery
- Dickens Heath Medical Centre
This ensures we are able to prioritise our focus on patients being able to access us through our telephone system when the demand is at its highest and support improving patient access for the majority of patients.
All sites will continue to be closed on Wednesdays from 12:30pm to 1:30pm, as part of our ongoing staff training and development, which is a priority to ensure we continue to improve service delivery and patient care. We are also dedicated to continuing to further upskill our Care Navigators with a programme of additional training and development to support our clinicians, and to ensure our patients see the right healthcare professionals at the appropriate time.
Our telephone lines remain open throughout the training and in the event of urgent patient needs, we can still be contacted. There is minimal impact on service delivery and no impact on appointments. This time has been chosen to coincide with the period of the day when our Doctors and healthcare professionals are conducting essential face-to-face appointments with housebound patients.
Please be polite and respectful, our GPs and practice teams are available and working hard to support you, your family and friends health and care needs.
Go online
Online services currently provide patients with access to their medical records, repeat medication ordering and COVID-19 vaccination status. Using the service will help you to manage your own health and access healthcare features whenever you need to.
You can visit our web site, and order repeat prescriptions and access your medical records on the NHS App and Patient Access – To access and find out more visit: https://solihullhealthcarepartnership.nhs.uk/online-services/
Our Online Consult facility is currently unavailable for patient safety online and clinical governance reasons. We are in the process of reviewing our online services to improve patient access and services, and will keep patients updated via our web site and social media.
Did you know?
You can visit your local pharmacy (Find a pharmacy - NHS (www.nhs.uk) for clinical advice on minor health concerns.
And for urgent issues or out of hours, you can also call the NHS on 111 or go online to seek NHS advice 111.nhs.uk (NHS 111 online)
Our staff are continuing to work extremely hard to provide services and care, and we would like to thank our patients for your continued support.
#HelpUsHelpYou
SURGERY CLOSURE FOR TRAINING:
Solihull Healthcare Partnership (SHP) Patient Participation Group (PPG) Update:
Patient involvement, engagement and communication is of utmost importance to Solihull Healthcare Partnership (SHP); in order for us to work together to improve patient outcomes and experience of the services we deliver.
SHP has a single PPG that covers all of our sites, with a growing membership and exciting plans for the future. The Chair and Secretary of the PPG also join our Board meetings on a monthly basis.
By definition, a PPG is a group of patients, carers and GP practice staff who meet to discuss practice issues and find a way forward, together. The patients’ voice is paramount and SHP fully recognise this and support collaborating with our patients.
SHP is a single practice with a single SHP PPG. We share the national vision of the PPGs purpose, including;
- To act as a critical friend
- To give patients and practice staff the opportunity to meet and discuss topics of mutual interest.
- To provide a means for patients to become more involved and make suggestions about the healthcare services they receive.
- To explore issues from patient complaints and patient surveys, contribute to action plans and help monitor improvements.
- To contribute feedback to the practice on National Patient Survey results and Friends and Family Test feedback to propose developments or change.
- To support health awareness and patient education
We welcome new members to join the SHP PPG and any anyone who would like to get involved can join via our website at https://solihullhealthcarepartnership.nhs.uk/patient-participation-group/